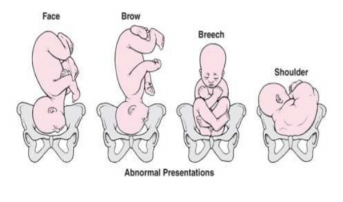
A caesarean section might be considered for the following reasons: 1. Abnormal lie: Under normal conditions, a baby lies head down in preparation for delivery. On occasion, a baby may be positioned abnormally, which necessitates an alternative to vaginal delivery.
NORMAL – baby is in a head-down position with the chin tucked in tightly
2. Breech: This involves the baby lying with its head at the top and bum at the bottom, or with its bum closest to the mother’s pelvis. As the baby is not positioned head first, a breech will complicate vaginal delivery
3. Face presentation: The baby passes through the pelvis face first. The baby’s head is not flexed – that is, the chin is not tucked in – so the head cannot easily descend and pass through the pelvis
4. Brow presentation: The brow presents at the pelvic brim. The baby’s head is not as flexed as it should be, which makes passage through the pelvis difficult
5. Transverse: The baby is lying sideways in the uterus, similar to the shoulder presentation illustrated below. A shoulder presentation or transverse lie occurs when the shoulder of the baby is in the pelvis, and the baby cannot be turned and delivered
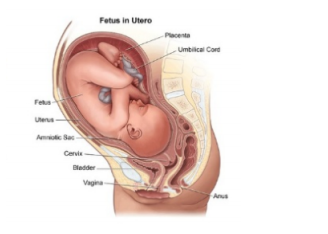
6. Placenta previa: The placenta lies very low or covers the cervix and prevents the baby from being delivered normally
7. Pregnancy-induced hypertension (PIH): Hypertension (high blood pressure) in pregnancy is also known as pre-eclampsia or pre-eclamptic toxaemia (PET) – If your blood pressure is very high, your doctor may recommend a caesarean section as a safer alternative
8. Gestational diabetes: Diabetes in pregnancy – some women will develop diabetes during their pregnancy. A caesarean section may also be recommended under such conditions if the baby has grown too big
9. Prematurity: A baby born before 37 weeks is known as a premature baby. Prematurity can be subcategorised further as follows:
Extremely preterm (<28 weeks)
Very preterm (28 – <32 weeks)
Moderate preterm (32 – <34 weeks)
Late preterm (34 – <37 weeks)
Early term (37 – <39 weeks)
Full term (39 – <41 weeks)
Late term (41 – <42 weeks)
Post term (42+ weeks)
There is a greater likelihood that a premature baby will be delivered by caesarean section, but this will depend on a number of factors that your doctor will advise you on accordingly
10. Multiples: A caesarean section may be required for multiple births. Twins may occasionally be born by normal vaginal delivery, but triplets and quadruplets will usually be born by caesarean section
11. Placenta abruption: The entire placenta, or a part of it, tears loose from the uterus
12. Cephalic pelvic disproportion: The baby is too large to pass through the mother's pelvic opening
13. Foetal distress – During a normal delivery, the baby may occasionally become tired or require emergency intervention
14. Unforeseen emergencies Hospital admission:
If your caesarean is planned or is an emergency, and caesarean birth becomes part of the birth plan, you may feel afraid or confused, or experience a multitude of different emotions. Along with joy at the imminent arrival of baby, there may also be disappointment and fear.
All hospitals have their own journey for the mother and her partner – starting from when you book in and finally arrive for the big day.
In general, the process is as follows:
1. As a mother-to-be, you will be admitted and prepared for theatre in the unit
2. You will be fetched from the unit and be taken to the theatre complex in your hospital bed
3. At theatre, you will be handed over to the theatre staff, and they will ask you some additional questions. They will also show your partner where to change
4. After waiting for a short while in the theatre reception area, you will be wheeled into theatre, and will be transferred onto the theatre table. Depending on the type of anaesthetic, your partner will most likely be able to stay with you at all times, but may be asked to wait outside at various stages
5. In order for the operation to be performed, you will need a small tube, known as a urinary catheter, placed in your bladder to drain the urine. In addition, an ‘IV’ line or ‘drip’ will be inserted – this is a small cannula placed in a vein which allows for fluids and medications to be administered. Depending on your hospital of choice, this placement might occur in either the unit or in theatre
6. An anaesthetic is now administered – this is either general or regional. A general anaesthetic is used to induce sleep for the duration of the procedure. A spinal block is a regional anaesthetic. This particular anaesthetic is injected into the fluid surrounding the spinal cord. While seated on the edge of your bed, the anaesthetist will administer a small numbing drug directly to your back. Thereafter, the anaesthetist will insert a needle into the space around your spinal cord and inject drugs to numb you from your waist down. Nothing is left in place in your back and the effect is near-instantaneous.
Some women may have had an epidural performed already as they may have been in labour and now require a caesarean section. An epidural and spinal anaesthetic are performed in the same way – but with an epidural, a very thin catheter is left in the back and drugs can be constantly administered through this. When you go for a caesarean, the epidural may be topped up to ensure you have no pain and the catheter will only be removed after the procedure
7. The scrub nurse will then start to clean your abdomen and apply sterile drapes
8. Keep one hand on your chest in order to be able to touch and hold your baby after the delivery
9. Remember that there will be a number of people in the theatre assisting with the delivery. They all have a role to play and this is quite normal
10. Do not touch the sterile theatre drapes and ensure that your hands remain beneath them. Your partner will be shown where to sit – and what he can touch
11. Your gynaecologist will now deliver the baby. You may feel some pressure but you will not feel any pain. From when your doctor starts the operation, it will be approximately 3–5 minutes until your baby is born
12. Once the baby is born, you will be able to see him/her. Depending on your hospital of choice, the baby will be examined by a paediatrician to confirm that he/she is in good health. Thereafter, you will be allowed to hold the baby
13. At a later stage, the baby will receive a Konakion (vitamin K) injection, and two identification bands will be applied. The baby will then be dressed and handed back to you or your partner to begin bonding
14. If there are any concerns about the baby, the paediatrician will discuss these with you. Please note that the baby may be taken to an area for monitoring if needed
15. When the doctor is finished with the operation, you will be moved back onto the unit bed and wheeled to the recovery room. Depending on each individual hospital’s setup and doctors’ preferences, the baby may stay with you or be taken to the nursery where you will be reunited once you leave the operating complex. In the recovery room, you will be checked for any bleeding, and your blood pressure and general condition will also be assessed
16. After confirming that all is well with you, your baby will be transferred back to the unit. The procedure takes approximately 1–2 hours from the time that you leave the unit until the time that you and your baby return
17. You can now have something to drink. You will be on a clear fluid diet at first to make sure your bowels are working, then a soft diet as prescribed by the doctor
18. Observations will be carried out regularly to ensure that you are well, and checks of your uterus and bleeding will be done regularly. These procedures will initially be frequent, but will gradually taper off as time passes. Your baby will be weighed and measured, and will be examined again. Additionally, a blood sugar check will be conducted, which involves a quick heel prick and blood drop
19. Breastfeeding will be encouraged and commenced as soon as possible after birth. We encourage rooming-in so that your baby can stay in your room next to your bed
20. The drip and catheter will normally be removed after a certain amount of time. Thereafter, you will be encouraged to get up, with assistance, and have a shower
21. It is important to walk around at regular intervals, and rest as much as you can in between
22. Pain management post-op will be explained by the doctors and nurses, and it is important to take this as prescribed. Some hospitals may use a small pump that allows you to manage your pain; alternatively, painkillers will be administered intermittently.
